Utilization Coaching
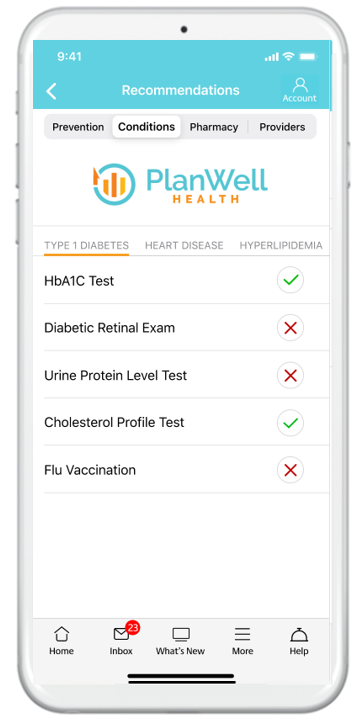
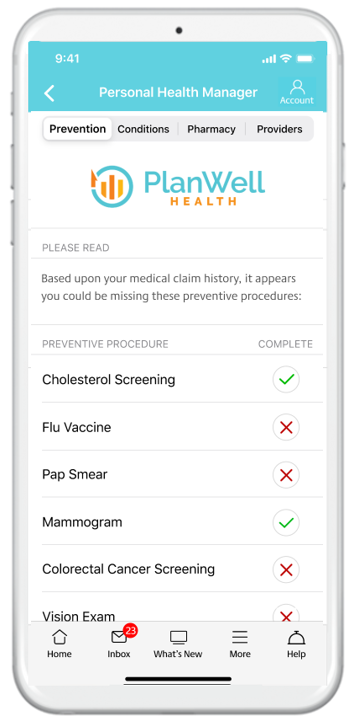
PlanWell automatically scans gaps in care and low quality providers, providing a coaching report card to healthplan members.
Understanding and navigating the U.S. health system can be very complicated and ultimately leaves many of your healthplan members confused on what care and providers to access. PlanWell Health utilization coaching helps simplify things.
We begin by leveraging your plan claim data analytics through our integration with Self Insured Reporting, accessing all of your members health plan claim data and metrics. Next we scan for opportunities of improvement and personalize these insights on behalf of each plan member.
We then deliver a monthly coaching report to each member showing simple ways they can take different actions and achieve better health outcomes.